Will the Coronavirus Pandemic Ever End?
After two years of fighting COVID-19, the end could be in sight.
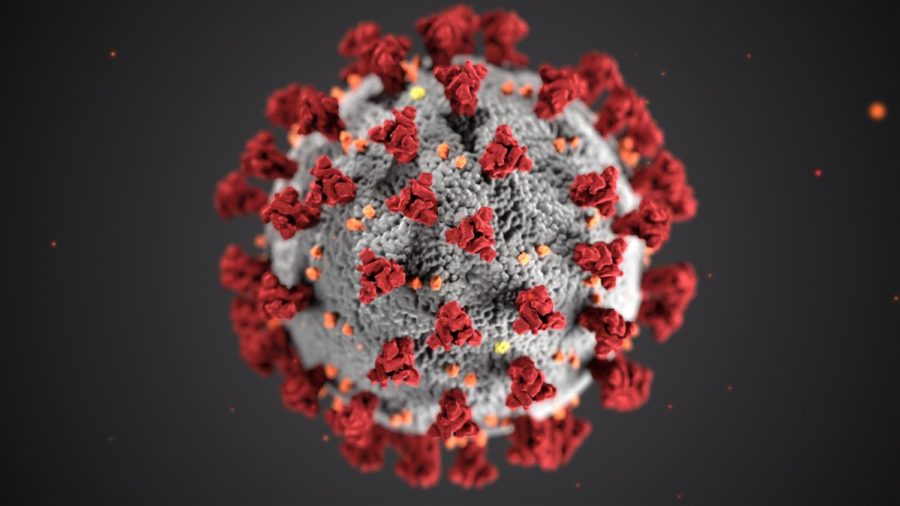
A computer rendition of a COVID-19 pathogen shows an up close detail of the virus that has caused a global pandemic.
On December 12th, 2019, a group of people in Wuhan, China fell sick to a mysterious, flu-like disease. Now, after two years, the virus has infected over 270 million people worldwide and claimed the lives of nearly 5.5 million people worldwide.
However, after a long battle with COVID-19, the tides seem to have turned: schools and workplaces have reopened in the United States and much of Europe, international travel has partially resumed, and 56.6% of the global population (roughly 4.4 billion people) have received at least one dose of the vaccine.
While everyday life seems to slowly return to “normal,” the long sought “end of the pandemic” seems to be nowhere in sight, especially with the rise of the Omicron variant. In fact, statistically, there has been little change at all. November 30th, 2020 marked the start of one of the deadliest COVID-19 waves seen in the United States, with an average of 1,270 deaths per week. Exactly a year later, on November 30th, 2021, that average rose to 1,555.
“[Statistics and real life] are two distinct aspects of the current situation and cannot be linked directly,” explains Xiaoyu Che, an assistant professor of biostatistics at the Columbia University Medical Center. “The statistical aspect is only influenced by the characteristics of the virus and by the public health measures, while…people’s lives [are] influenced by a wide range of factors, e.g., economics, politics, and are subjective, etc.”
What this means is every-day life could change drastically while statistics remain the same. The constantly interchanging aspects of life makes it difficult to properly answer the question: Will the pandemic end? “[Life] is [too] complicated to quantitatively analyze,” elaborated Che. This implies life could “return to normal,” even while COVID-19 lingers.
Variable aspects such as changes in people’s life-styles makes the question of how, when, and even if the pandemic will end a debated topic. Neither epidemiologists, topic researchers, biostatistic analysts, or other experts can find a definitive answer – or agree on one.
All attributes of the world such as human behavior, air humidity, and even wind patterns affect the COVID-19 pandemic. With this many factors at play – and at such a large scale – tasks such as creating vaccines, suppressing outbreaks, and disease forecasting become difficult.
“Many factors that determine the future of the pandemic are uncertain,” said Sen Pei, an assistant professor of environmental health sciences at the Columbia Mailman School of Public Health. “The emergence of Variants of Concern (VOC) and their ability to escape immunity are hard to predict, and they are constantly shaped by shifting human behavior.”
“[COVID-19] spreads…efficiently…and mutates more than we would have hoped,” elaborated Dr. Tracy LaGrassa, a teacher of cell biology at The Bronx High School of Science. “Its [attributes] allow it to evade our immune defenses…The virus’ nature means that we’ve got to wait and see with the science.”
While there are large levels of uncertainty surrounding the future of the COVID-19 pandemic, researchers and scientists aren’t completely at loss. Using data analytics, extensive trials, and knowledge from previous pandemics, they can formulate probable ideas.
A common speculation is that we won’t completely “erase” COVID-19, but we will learn to live with it. This situation could be similar to the 1918 Spanish Flu pandemic which killed roughly 50 million people before “disappearing” and “reappearing” as the less vehement strain we now call the seasonal flu.
“The most likely outcome is that [the] COVID-19 pandemic will end and become like the flu, [an] endemic…recurring each year,” said Professor Charles Branas, a Gelman Endowed Professor and Chair for the Department of Epidemiology in Columbia University Mailman School of Public Health. “We’ll adapt our vaccines and our behavior (maybe even wearing masks more often) over the years.”
An endemic is where a disease is “contained” and contracted within a specific location. Experts, such as Professor Branas, predict that with vaccines, mask-wearing, and social distancing, the pandemic will eventually “simmer down” to a – much less deadly – localized “endemic.”
Journalist Paul Hunter at The Prevention Web elaborates the possibility of an endemic in his article ‘How Will the COVID Pandemic End?’ “While vaccines do reduce transmission, they don’t block infection to a high enough degree to eradicate the virus. Even before the Delta variant arrived, we were seeing double-vaccinated people both catching the virus and spreading it to others…Because immunity to infection is neither absolute nor permanent, herd immunity is unachievable. What this means is that COVID-19 is likely to become endemic.”
However, some specialists like Dr. Mark Dybul, a professor in the Department of Medicine for Georgetown University, questions if the “end” is truly guaranteed for the near future. “I think by March, April, May, we will have a fully vaccine-resistant variant,” he said at the Fortune CEO Initiative conference in Washington, D.C. “There’s simply no way you can have such low rates of vaccination around the world with the virus ping-ponging between vaccinated and unvaccinated people…The probability of us seeing a vaccine-resistant strain is very high.”
Days after Dr. Dybul said this, the world discovered the Omicron strain in South Africa. “Omicron is likely to be the most infectious SARS-Cov-2 variant to date ([it can] spread twice as quickly as Delta),” explains Che. He believes that – although concerning – the Omicron variant isn’t something to panic about. “Data [suggests] that diseases caused by Omicron infections might be less serious than other forms of the virus. The Omicron variant can still be detected using the current PCR [polymerase chain reaction, better known as a COVID-19 (non-rapid) test] assays; … the Pfizer vaccine can increase the [chance of] neutralizing [Omicron] 25-fold… ; and the new antiviral pills from Merck and Pfizer should still be effective against Omicron.”
Though it is fortunate Omicron hasn’t mutated into a more deadly strain, “curve balls” like these have – and will continue to lessen the world’s ability to end the pandemic.
Dr. Erin O’Leary, a teacher of epidemiology at The Bronx High School of Science, elaborates on why COVID-19 is so hard to effectively combat. “The majority of people throughout the world do not have immunity to this virus. Therefore, the only ways to achieve immunity to the virus are by infection or vaccination. What makes it difficult to suppress is that many people who are infected do not have symptoms, and can unknowingly transmit it to other people.”
In addition to vaccine-resistant strains, cross-infection from human to animals risks hindering our ability to stop the spread of the virus. A New York Times study in November 2021, indicated that roughly 80 percent of white-tailed deer in Iowa had contracted COVID-19. While there haven’t been any confirmed cases of the deer re-transmitting the virus to humans, it’s very possible. It only takes one transmission to cause an outbreak, and – as the virus’s two-year history has proven– an outbreak can lead to devastating consequences.
While some specialists debate the future of the pandemic on a “spectrum” of exposure, others , such as Professor Nick Wilson, a specialist in the Department of Public Health for the University of Otago, believe the world should not dismiss the possibility of eradicating COVID-19 entirely.
“Global eradication of COVID-19 is not out of the question…because we seem to have the available tools,” he said. “We have effective vaccines and a range of public health and social measures that have been shown to work at a country-level. What the world seems to lack is the political will to use these tools appropriately.”
While this topic remains largely uncertain, there is one fact that is guaranteed: it will take a while to create a definitive answer as to what will happen, and even longer to reach it. Especially with an unpredictable virus like COVID-19, variants (like the Omicron variant), vaccine hesitancy, and waning immunity all prove overcoming this global pandemic will take a global effort. The international communities will need to work together to tackle a problem of such magnitude.
However, humans have successfully ended pandemics before. Now with modern technology, we have more capability than ever. “It has been done before,” said Dr. LaGrassa. “We can definitely do it [again].”
“Global eradication of COVID-19 is not out of the question…because we seem to have the available tools…What the world seems to lack is the political will to use these tools appropriately,” said Professor Nick Wilson, from the Department of Public Health at the University of Otago.
Oliver Whelan is an Editor-in-Chief for ‘The Science Survey.’ He enjoys journalistic writing because of its ability to convey information on topics...